Advocacy for infant and early childhood mental health (Links to an external site)



Starting a new school year can be stressful for all members of the household. While the return to school will be exciting for some students (and maybe a welcome change for parents), others may be feeling anxious or frightened about heading to school for possibly the first time or attending a new school. Here are […]
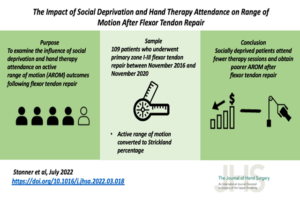
Milliken Hand Rehabilitation Center Hand Therapists, Macy Stonner, OTD, OTR/L, CHT & Logan Berlet, OTD, OTR/L were recently published in The Journal of Hand Surgery for their paper, “The Impact of Social Deprivation and Hand Therapy Attendance on Range of Motion After Flexor Tendon Repair.” The purpose of the paper was to examine the influence […]

June 6 – 10th, our Milliken Hand Rehabilitation Team participated in activities and challenges celebrating the annual Hand Therapy Week led by the American Society of Hand Therapists. Some of the unique ways that we were able to highlight our talented team was by showcasing “blinged-out” orthotic creations, getting the thoughts of a hand therapist […]
Occupational Therapy is a profession that assists people throughout their lifetime and believes that participation in daily activities (aka occupations) is vital to mental health and well-being. Your Washington University Occupational Therapist may help you utilize familiar activities as coping mechanisms, such as listening to music, playing cards, writing, doodling, cooking, or cleaning to help provide calming […]

Washington University Occupational Therapy works with many healthcare providers, physician groups, living facilities, and community organizations to provide the best care, When & Where our patients need it most. During the month of April, we will be celebrating OT Month and promoting all that our providers and colleagues in the field do for our adult and pediatric […]

Washington University Occupational Therapy works with our patients on self-management and self-care all year-round. With February being American Heart Month we want to promote self-care heart-healthy tips for your daily routine. Below are some actions that you can include in your routine; These few basic tips will help you begin or refocus on your journey toward […]

The age-old question that actors have been asking Directors… This phrase directly applies to everyone as we take on a new year. Are you motivated this year to pursue new health goals, career objectives, or personal initiatives? Motivation is the beginning of all choices.

Thanksgiving only comes around once a year, so why not go ahead and splurge? Year after year, we can all attest that during the holidays thinking about healthy eating may not be our primary consideration. But Thanksgiving does not have to sabotage your diets. With a little self-control, we can satisfy our desire for traditional […]

Some years are more special than others in the life of a clinic, this happens to be the case for the Milliken Hand Rehabilitation Center in 2021. This year marks the 50th anniversary of Milliken and its dedication to helping hands and working with physicians to provide outstanding patient care. To honor this milestone a […]

Washington University Occupational Therapist & Instructor, Sue Tucker, OTD, OTR/L, ATP is an Assistant Coach for USA Wheelchair Rugby (USAWR), and this past week Sue was helping guide the team as they played on the big stage in the Paralympic Games Tokyo 2020! The USAWR Team had an outstanding showing at the Paralympic Games Tokyo […]
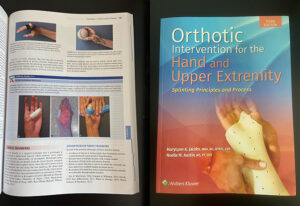
The third edition of ‘Orthotic Intervention for the Hand and Upper Extremity’ was published this year and is recently in print. New to this edition is a chapter devoted to nerve and tendon transfers. The editors reached out to therapists at Milliken Hand Rehabilitation Center at Washington University to write this chapter given the national […]
Occupational therapy’s goal is to help patients utilize their strengths, maximize their potential, and counteract their limitations to help them meet their goals. As we continue to see rising numbers of COVID-19 cases, our team is here to work with patients recovering from the physical and emotional challenges patients may be facing from the virus. […]

We all love summer as it brings warm weather and outdoor activity. Summer injuries are a common reason to seek medical care. However, with proper caution and planning, save yourself a trip to the emergency room! Have fun this summer, but keep yourself and others away from summer injuries. If you sustain an upper-extremity injury, […]
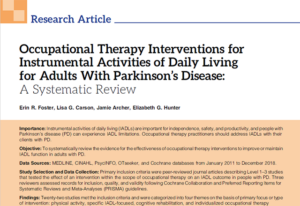
Our Clinic Manager, Jamie Archer, MOT, OTR/L was recently published for her work on Occupational Therapy Interventions for Instrumental Activities of Daily Living for Adults With Parkinson’s Disease: A Systematic Review. Congratulations to Jamie and her colleagues for their work and recent publication in the American Journal of Occupational Therapy (AJOT). Click here or the […]

June 7th – 13th we will recognize our Hand Therapists during the American Society of Hand Therapists (ASHT) Hand Therapy Week. This highly specialized group of therapists provide patient care at the Milliken Hand Rehabilitation Center. The Milliken Hand Rehabilitation Center was one of the first three hand rehabilitation facilities established in the U.S. With […]

Here are some tips and strategies to help with mental fatigue:

Washington University Occupational Therapy works with many healthcare providers, physician groups, living facilities, and community organizations to provide the best OT care, When & Where our patients need it most. During the month of April, we will be celebrating our OT providers and colleagues and all that they do for our adult and pediatric patients. […]
Washington University Occupational Therapy works with our patients on self-management and self-care all-year-round. With February being American Heart Month we want to promote self-care heart-healthy tips for your daily routine. Below are some actions that you can include in your routine;

In 2020 our Therapists provided their expertise to the following Clinical Publications & Journals: Citations: Berlet, L., & Kaskutas, V. (2020). Developing occupation kits in a Hand Therapy Student Experiential Learning Clinic. Hand Therapy, 25(2), 73-82. Cochrane, S. K., Calfee, R. P., Stonner, M. M., & Dale, A. M. (2020). The relationship between depression, anxiety, and pain […]

This month we are highlighting and giving a special congratulations to one of our Pediatric Therapists, Karen Balk, MOT, OTR/L. Karen presented her pediatric research work on GNAo1 disorders internationally earlier this month. Karen’s pediatric research presentation on patients with GNAo1 disorder and gene mutations was attended by roughly 160 attendees from 20 different countries […]

Washington University Occupational Therapy operates a student-run stroke clinic with the guidance and oversight of licensed Occupational Therapists. The clinic offers free services for under-resourced patients to help increase safety and independence for people following a stroke. We work to empower our patients and families by providing them with the knowledge and tools they need […]

Are you working with patients or community members that are wanting to make goals for themselves or focused on improving their sense of wellbeing and their overall ability to manage life’s transitions? Washington University Occupational Therapy is collaborating with Aging Ahead on an 8 – week Map Your Path To Well-Being Program. Topic areas discussed […]

Summer is a time for us to relax and take a load off of our brains that we’ve been putting to heavy use throughout the academic year. But for children with executive dysfunction, the long summer break with a lack of structure can hurt their brains’ ability to maintain what they just learned in school, […]

View our Firework Safety Tip Sheet The summer of 2020 is different from any we have known before. Covid-19 has affected our ability to celebrate with the normal parades, gatherings, and summer celebrations. Large firework displays have been canceled this year. This may lead to more inexperienced people handling fireworks meaning Fireworks & Hand Safety […]

June 1st – 7th we will recognize our Hand Therapists during the American Society of Hand Therapists (ASHT) Hand Therapy Week. This highly specialized group of therapists provide patient care at the Milliken Hand Rehabilitation Center. The Milliken Hand Rehabilitation Center was one of the first three hand rehabilitation facilities established in the U.S. With […]

5 ways OT can help build a Healthier, Happier “You” in 2020! Learn more about our services…
With November being National Diabetes Awareness Month, the timing seems appropriate to talk about Washington University Occupational Therapy and how our chronic disease self-management services provide strategies, behaviors, and principles to help patients who are experiencing life with diabetes both Type 1 or Type 2. Occupational therapy services are valuable in the management of many […]

Do you or your colleagues treat patients that suffer from pain in their hands? Join us as we host the American Society of Hand Therapists and their traveling course, “Beating Pain.” This full-day course will review contemporary pathophysiological mechanisms underlying pain. Using insights into the somatosensory experience of pain, specific assessments and treatment strategies will […]
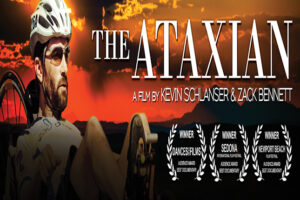
Unable to walk due to the neuromuscular disorder, Friedreich’s ataxia (FA), Kyle Bryant and a team of friends attempt the most grueling bicycle race in the world, The Race Across America (RAAM). The feature-length documentary, “TheAtaxian,” spotlights a man whose will and determination carry him and his teammates across a continent under almost impossible conditions-an […]

Earlier this month Washington University Occupational Therapy received the opportunity to host and provide a lecture for the St. Louis College of Pharmacy BESt Summer Institute. Duana Russell-Thomas, OTD, OTR/L gave an insightful look into the field of Occupational Therapy as a profession. The BESt program has been designed to provide local rising high school […]

June is Alzheimer’s and brain awareness month. One reason we promote awareness of brain health is that some forms of dementia are preventable. Alzheimer’s disease is not a normal part of aging. Just like other parts of our body, the brain needs care, exercise, and attention.