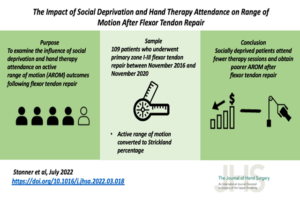
While the work began in 2020 Milliken Hand Rehabilitation Center, Hand Therapist, Stacy Baker, MOT, OTR/L, CHT recently learned her work with Washington University School of Medicine in St. Louis and St. Louis Children’s Hospital colleagues was recently published in the Journal of Hand Surgery Global Online. The purpose of the article was to look […]
Milliken Hand Therapist Part of Team Published in Journal of Hand Surgery Global Online